Critical Analysis: Top 3 US Healthcare Challenges in 2025

Critical Analysis: The 3 Biggest Challenges Facing the US Healthcare System in 2025 include rising costs, access disparities amplified by social determinants of health, and the integration of technology while maintaining patient privacy and data security.
Navigating the future of healthcare in the United States requires a sharp focus on the hurdles that lie ahead. Let’s dive into a critical analysis: the 3 biggest challenges facing the US healthcare system in 2025.
Critical Analysis: Rising Healthcare Costs
One of the most pressing concerns is the relentless increase in healthcare costs. This challenge affects individuals, employers, and the government.
The escalating expenses are driven by several factors.
Drivers of Cost Increases
Technological advancements, while improving treatment options, often come with a hefty price tag. New drugs, sophisticated diagnostic tools, and innovative procedures contribute to higher overall costs.
An aging population also adds to the financial strain. Older adults typically require more medical care and long-term services, increasing demand and expenses.
- Administrative overhead: Streamlining administrative processes could yield significant savings.
- Drug pricing: Negotiating drug prices and promoting generic alternatives can reduce costs.
- Preventive care: Investing in preventive measures can lower the need for costly treatments later.
Addressing rising healthcare costs requires a multi-pronged approach, including policy changes, technological innovations, and a shift towards value-based care.
Critical Analysis: Healthcare Access and Disparities
Ensuring equitable access to healthcare remains a significant challenge. Disparities based on race, ethnicity, socioeconomic status, and geographic location persist across the US.
These disparities are often rooted in broader social determinants of health.
Social Determinants of Health
Factors such as poverty, lack of education, inadequate housing, and food insecurity significantly impact health outcomes. Individuals facing these challenges often experience barriers to accessing timely and quality healthcare.
Geographic location also plays a crucial role. Rural areas often lack healthcare facilities and providers, making it difficult for residents to receive necessary care.
- Expanding Medicaid: Increasing eligibility and enrollment in Medicaid can improve access for low-income individuals.
- Community health centers: Supporting community health centers can provide care in underserved areas.
- Telehealth: Leveraging telehealth technologies can bridge geographic barriers and improve access to specialists.
Reducing healthcare disparities requires addressing the underlying social and economic factors that influence health outcomes. Targeted interventions and culturally sensitive approaches are essential to ensure equitable access for all.
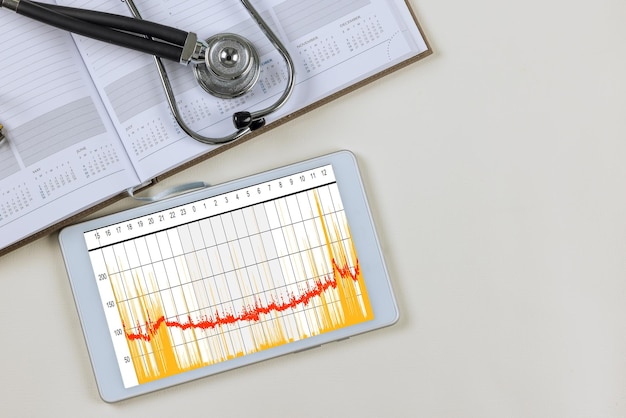
Critical Analysis: Technology Integration and Data Security
The increasing reliance on technology in healthcare presents both opportunities and challenges. While digital tools can enhance efficiency and improve patient care, they also raise concerns about data security and privacy.
Integrating technology into healthcare requires careful planning and implementation.
Enhancing Efficiency and Patient Care
Electronic health records (EHRs) can improve care coordination and reduce medical errors. Telehealth platforms can expand access to care, particularly for patients in remote areas.
Artificial intelligence (AI) and machine learning (ML) have the potential to revolutionize diagnostics and treatment. These technologies can analyze vast amounts of data to identify patterns and predict health outcomes.
- Cybersecurity measures: Healthcare organizations must invest in robust cybersecurity measures to protect patient data.
- Data privacy regulations: Strengthening data privacy regulations can safeguard patient information and promote trust.
- Ethical considerations: Addressing ethical considerations surrounding AI and ML in healthcare is crucial to ensure responsible use.
Addressing data security and privacy concerns is paramount to maintain patient trust and realize the full potential of technology in healthcare. Balancing innovation with patient protection is essential.
Critical Analysis: The Impact of Policy and Regulation
The US healthcare system is heavily influenced by policy and regulation. Changes in these areas can have a significant impact on costs, access, and quality of care.
Understanding the role of policy and regulation is crucial.
Policy and Regulatory Changes
The Affordable Care Act (ACA) has expanded health insurance coverage to millions of Americans. However, ongoing debates about its future create uncertainty for the healthcare industry.
Regulatory policies, such as those related to drug pricing and insurance practices, can significantly affect healthcare costs. Changes in these policies can have far-reaching consequences for patients and providers.
- Bipartisan solutions: Finding bipartisan solutions to address healthcare challenges is essential for long-term stability.
- Evidence-based policymaking: Relying on evidence to inform policy decisions can lead to better outcomes.
- Stakeholder engagement: Engaging stakeholders, including patients, providers, and insurers, in the policymaking process can ensure that policies are effective and sustainable.
Navigating the policy and regulatory landscape requires staying informed and advocating for policies that promote affordable, accessible, and high-quality healthcare.
Critical Analysis: The Evolving Role of Healthcare Providers
Healthcare providers are at the forefront of addressing the challenges facing the US healthcare system. Their roles are evolving in response to changing patient needs and technological advancements.
Providers are adapting to new models of care.
Adapting to New Models of Care
The shift towards value-based care emphasizes quality and outcomes over volume. Providers are increasingly being incentivized to deliver efficient and effective care.
Team-based care models, which involve collaboration among physicians, nurses, and other healthcare professionals, can improve care coordination and patient outcomes.
- Workforce training: Investing in workforce training and development can ensure that providers have the skills and knowledge needed to succeed in a changing healthcare landscape.
- Burnout prevention: Addressing provider burnout is crucial to maintain a high-quality and engaged workforce.
- Technology adoption: Supporting providers in adopting and using new technologies can improve efficiency and patient care.
Empowering healthcare providers and supporting their professional development is essential to ensuring a sustainable and high-quality healthcare system.
Critical Analysis: The Future of US Healthcare
The future of US healthcare will be shaped by the choices we make today. Addressing the challenges discussed above requires a concerted effort from policymakers, providers, and the public.
A collaborative approach is essential.
A Collaborative Approach
Investing in preventive care and promoting healthy lifestyles can reduce the burden of chronic diseases. Addressing social determinants of health can improve health outcomes and reduce disparities.
Leveraging technology to improve efficiency and enhance patient care is crucial. Protecting patient data and ensuring privacy are essential for maintaining trust.
- Public health initiatives: Supporting public health initiatives can improve population health and reduce healthcare costs.
- Community partnerships: Building community partnerships can address social determinants of health and improve access to care.
- Innovation and research: Investing in innovation and research can lead to new treatments and technologies that improve health outcomes.
By working together, we can create a healthcare system that is affordable, accessible, and equitable for all Americans.
| Key Point | Brief Description |
|---|---|
| 💰 Rising Costs | Healthcare costs continue to rise, impacting individuals and the government. |
| 🩺 Access Disparities | Unequal access to healthcare persists due to socio-economic factors. |
| 🔒 Tech & Security | Balancing technology integration with data security is a key challenge. |
| 🏛️ Policy Impact | Policy changes greatly influence healthcare costs and access. |
FAQ
▼
The primary drivers include technological advancements, an aging population, administrative overhead, and high drug prices. Addressing these factors is crucial for cost containment.
▼
Social determinants, like poverty and lack of education, create barriers to accessing quality healthcare. These factors contribute to health disparities among different populations.
▼
Implementing robust cybersecurity measures, strengthening data privacy regulations, and addressing ethical considerations related to AI are essential for protecting patient data.
▼
Policy changes, such as those under the Affordable Care Act, and regulations related to drug pricing and insurance practices significantly affect healthcare costs, access, and quality of care.
▼
Healthcare providers are adapting to new models of care, such as value-based and team-based approaches. Continuous training and preventing burnout are vital for their success.
Conclusion
In conclusion, the US healthcare system faces significant challenges in 2025, including rising costs, healthcare access disparities, and balancing technology integration with data security. Addressing these issues requires a collaborative effort from policymakers, providers, and the public to ensure a more affordable, accessible, and equitable healthcare system for all Americans.
